Filariasis remains one of the world’s most persistent neglected tropical diseases, affecting millions of people primarily in low-income regions with limited access to healthcare, sanitation, and infrastructure. Caused by mosquito-borne filarial worms such as Wuchereria bancrofti, Brugia malayi, and Brugia timori, the disease can lead to debilitating conditions like lymphedema and hydrocele, collectively known as lymphatic filariasis.
Although treatment options exist, the true engine of progress lies not in clinical care alone but in comprehensive public health interventions that target the disease at every stage of transmission. Public health systems play a multifaceted and indispensable role in reducing disease incidence, preventing lifelong disability, and breaking cycles of poverty that filariasis often perpetuates.
Understanding Filariasis as a Public Health Challenge
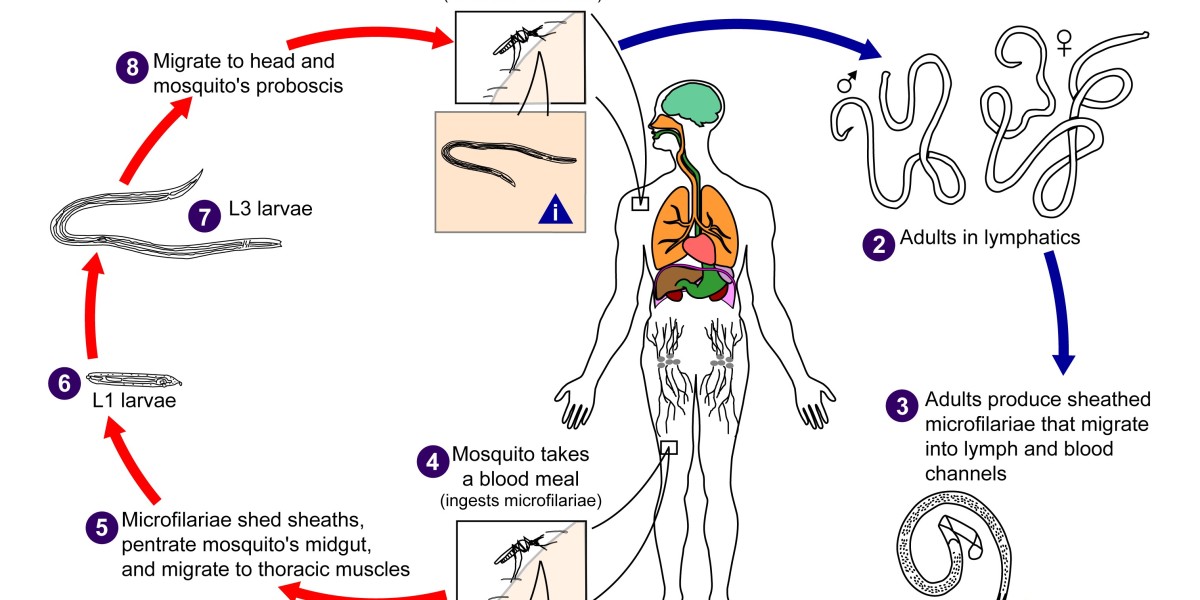
Filariasis is not merely a medical condition but a disease rooted in environmental, socioeconomic, and behavioral factors. Transmission relies heavily on mosquito vectors, which proliferate in areas with poor drainage, inadequate sanitation, and inconsistent waste management.
Communities with limited access to health education or preventive tools remain particularly vulnerable. Addressing filariasis therefore requires action that transcends the boundaries of hospitals and clinics it demands coordinated community-level, national, and global public health strategies.
Mass Drug Administration: A Cornerstone of Prevention
One of the most successful public health interventions against lymphatic filariasis has been Mass Drug Administration (MDA), in which entire at-risk populations receive antiparasitic medications to reduce microfilariae in the bloodstream. By lowering the parasite load in humans, MDA interrupts transmission to mosquitoes and subsequently to new hosts. The World Health Organization (WHO) recommends combinations of drugs such as ivermectin, diethylcarbamazine, and albendazole for large-scale distribution.
Although medications like mebendazole 500mg are used for various parasitic infections, the significance of MDA programs lies not in a single drug but in the coordinated, community-wide effort to suppress the parasite reservoir.
Public health agencies are responsible for planning drug distribution, educating communities on safety, training volunteers, and monitoring coverage levels to ensure that at least 65-80% of the population receives treatment annually for several consecutive years. Without such organized systems, individual treatment would have minimal impact.
Vector Control and Environmental Management
While drug administration deals with the human reservoir, vector control targets the mosquitoes that transmit filarial worms. Public health efforts in this area focus on reducing mosquito breeding sites and minimizing human-vector contact. Key strategies include
Environmental cleaning: removing stagnant water, improving drainage systems, and managing waste.
Larviciding programs: applying biological agents or environmentally safe chemicals to water bodies to reduce mosquito larvae.
Distribution of insecticide-treated nets (ITNs): providing communities with bed nets that offer protection during peak mosquito activity.
Indoor residual spraying: applying insecticides to walls and structures where mosquitoes rest.
These interventions require government coordination, funding, and community engagement. Vector control teams work with local leaders to implement sustainable practices, while surveillance systems measure mosquito density and transmission levels. Public health programs must adapt to local ecological conditions, acknowledging that the effectiveness of vector control varies by mosquito species and regional climate.
Health Education and Behavior Change
No public health initiative succeeds without community understanding and participation. Education campaigns form a critical component of filariasis control, helping individuals recognize symptoms, reduce stigma, and understand prevention measures. Public health educators use diverse approaches including school programs, radio messages, door-to-door outreach, and partnerships with local organizations to communicate essential information.
Behavior change strategies emphasize:
consistent participation in MDA programs,
proper use of bed nets and repellents,
environmental hygiene and waste disposal,
early reporting of symptoms.
By empowering communities with knowledge, public health systems promote shared responsibility and long-term disease reduction. Education also helps dispel misconceptions that often discourage treatment, such as fear of medication side effects or stigma surrounding swollen limbs.
Disability Prevention and Community Support
Even when transmission is reduced, many individuals already live with chronic complications of filariasis. Public health programs therefore integrate morbidity management and disability prevention (MMDP). These activities are designed to improve quality of life and prevent disease progression through:
hygiene training to reduce infection risk in swollen limbs,
management of acute inflammatory episodes,
promotion of exercise and limb elevation routines,
surgical interventions for hydrocele where resources allow,
establishment of support groups for affected individuals.
MMDP is not simply a medical service; it is a public health priority that helps restore dignity, functionality, and productivity. Communities benefit when stigma is reduced and affected individuals can participate fully in social and economic activities.
Surveillance and Data-Driven Decision Making
Public health is fundamentally data-driven. Effective filariasis control relies on accurate surveillance to identify risk areas, track infection patterns, and evaluate the impact of interventions. Programs use tools such as:
mapping surveys to identify endemic zones,
sentinel site monitoring to measure microfilaria prevalence,
transmission assessment surveys (TAS) to determine whether MDA can be discontinued,
laboratory diagnostics including antigen detection tests,
entomological surveillance to track mosquito infection rates.
Data allows public health agencies to allocate resources efficiently, modify strategies, and ensure that progress toward elimination targets remains on track. Modern technologies including mobile data collection, GIS mapping, and digital health platforms have further enhanced accuracy and responsiveness.
Global and National Partnerships
The fight against filariasis exemplifies the power of collaboration. International initiatives such as the WHO’s Global Programme to Eliminate Lymphatic Filariasis (GPELF) bring together governments, NGOs, donor organizations, researchers, and pharmaceutical companies. These partnerships enable resource pooling, standardized protocols, and large-scale drug donation programs that make MDA financially feasible for low-income countries.
At the national level, ministries of health coordinate campaigns that involve community workers, local leaders, and public health officers. Success depends on cooperation across sectors including sanitation, education, environmental management, and social welfare reflecting filariasis’s complex socio-environmental nature.
The Path to Elimination
Significant progress has been made: several countries have already achieved elimination as a public health problem, demonstrating that victory is possible. The path forward requires sustained political will, stable funding, robust surveillance, and continued community engagement. Public health agencies must balance elimination efforts with long-term care for those already affected, ensuring that no community is left behind.
Conclusion
Public health plays a pivotal role in combating filariasis by integrating scientific knowledge, community action, environmental management, and national policy. Through mass drug administration, vector control, health education, disability support, and global partnerships, public health systems address both the biological and social dimensions of the disease.
While treatments including antiparasitic agents referenced broadly in public health discussions, such as mebendazole 500mg have their place, it is the collective public health framework that enables long-term control and eventual elimination. By strengthening these systems, the world moves closer to a future where filariasis is no longer a burden on individuals, families, or entire communities.